Pain management doctors play a crucial role in the healthcare system by providing specialized care for patients suffering from chronic pain. These doctors are trained to diagnose and treat various types of pain, including acute, chronic, and cancer-related pain. They work closely with patients to develop personalized treatment plans that may include medication, physical therapy, and interventional procedures. Pain management doctors also play a key role in educating patients about their condition and empowering them to take an active role in managing their pain.
In addition to their clinical responsibilities, pain management doctors also collaborate with other healthcare professionals to ensure comprehensive care for their patients. They may work closely with primary care physicians, surgeons, physical therapists, and mental health professionals to address the multifaceted nature of chronic pain. By taking a holistic approach to pain management, these doctors can help improve the quality of life for patients and reduce the burden of chronic pain on the healthcare system.
Key Takeaways
- Pain management doctors play a crucial role in helping patients manage and alleviate their pain through various treatment methods.
- Narcotics are an important tool in pain management, but they should be used cautiously and responsibly due to their potential for addiction and abuse.
- Pain management doctors have a responsibility to carefully assess and monitor patients who are prescribed narcotics to ensure safe and effective use.
- Collaborating with patients is essential for successful pain management, as it allows doctors to understand the patient’s needs and adjust treatment plans accordingly.
- It is important for pain management doctors to openly discuss the risks and benefits of narcotic use with their patients to make informed decisions about their treatment.
- The future of narcotic prescribing in pain management will likely involve a more cautious and individualized approach to minimize the risks and maximize the benefits for patients.
The Importance of Narcotics in Pain Management
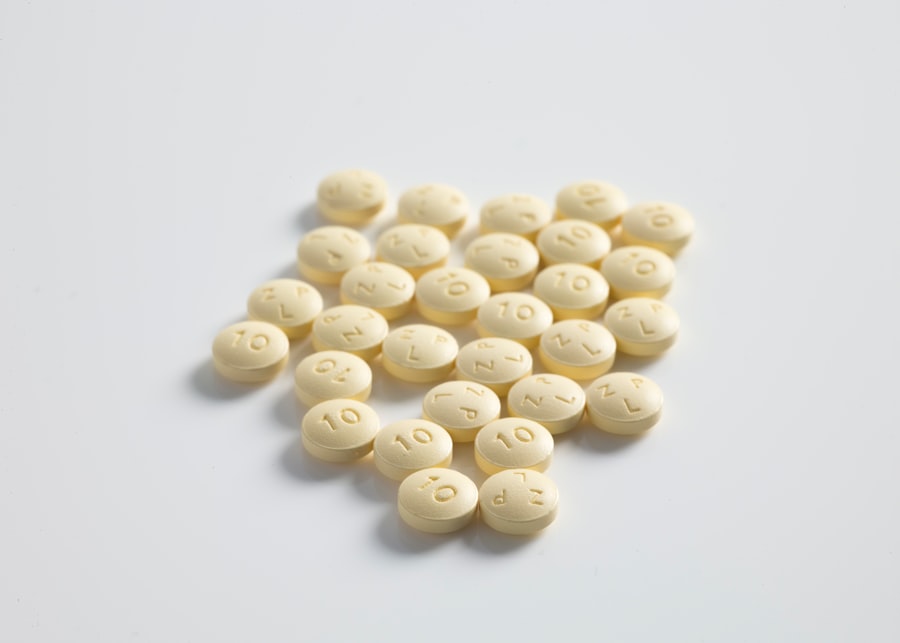
Narcotic medications, also known as opioids, play a crucial role in the management of moderate to severe pain. These medications work by binding to opioid receptors in the brain and spinal cord, effectively reducing the perception of pain. For patients suffering from chronic pain conditions such as cancer, neuropathy, or rheumatoid arthritis, narcotics can provide much-needed relief and improve their overall quality of life.
In addition to their analgesic properties, narcotics can also help improve function and mobility for patients with chronic pain. By reducing the intensity of pain, these medications can enable patients to engage in physical therapy and other rehabilitative activities that may have been previously too painful. This can ultimately lead to improved physical function and a greater sense of independence for patients with chronic pain.
Despite their effectiveness in managing pain, narcotics also carry a risk of abuse and addiction. Pain management doctors must carefully weigh the benefits and risks of prescribing narcotics for each patient, taking into account their medical history, current health status, and potential for misuse. By striking a balance between pain relief and risk mitigation, these doctors can help ensure safe and effective treatment for their patients.
The Responsibility of Pain Management Doctors in Prescribing Narcotics
Prescribing narcotics is a complex and multifaceted responsibility for pain management doctors. These healthcare professionals must carefully assess each patient’s unique needs and develop individualized treatment plans that prioritize safety and efficacy. This involves conducting thorough medical evaluations, reviewing medical records, and discussing the potential risks and benefits of narcotic use with patients.
In addition to their clinical responsibilities, pain management doctors must also stay informed about current guidelines and best practices for prescribing narcotics. This includes staying up-to-date on the latest research and recommendations from professional organizations such as the Centers for Disease Control and Prevention (CDC) and the American Society of Anesthesiologists (ASA). By adhering to evidence-based guidelines, these doctors can help minimize the risk of opioid misuse and addiction while still providing effective pain relief for their patients.
Furthermore, pain management doctors must also communicate openly and transparently with their patients about the use of narcotics. This includes discussing potential side effects, monitoring requirements, and alternative treatment options. By fostering a collaborative and trusting relationship with their patients, these doctors can help ensure that narcotic use is managed responsibly and in the best interest of the patient’s overall well-being.
Assessing and Monitoring Patients for Narcotic Use
| Patient Name | Pain Level | Narcotic Use | Monitoring Frequency |
|---|---|---|---|
| John Doe | 7/10 | Yes | Every 4 hours |
| Jane Smith | 5/10 | No | Every 6 hours |
| Michael Johnson | 8/10 | Yes | Every 2 hours |
Assessing and monitoring patients for narcotic use is a critical aspect of the role of pain management doctors. Before prescribing narcotics, these healthcare professionals must conduct thorough assessments to evaluate each patient’s medical history, current health status, and risk factors for opioid misuse. This may involve reviewing previous medical records, conducting physical examinations, and ordering diagnostic tests to better understand the nature and severity of the patient’s pain.
Once a patient has been prescribed narcotics, pain management doctors must also implement ongoing monitoring strategies to ensure safe and effective use of these medications. This may include regular follow-up appointments to assess the patient’s response to treatment, monitor for potential side effects, and adjust the treatment plan as needed. Additionally, these doctors may use tools such as urine drug testing and prescription drug monitoring programs to identify any signs of misuse or diversion.
In cases where patients are at higher risk for opioid misuse or addiction, pain management doctors may also consider implementing additional monitoring measures such as pill counts or referral to addiction specialists. By taking a proactive approach to assessing and monitoring patients for narcotic use, these doctors can help minimize the risk of opioid-related harm while still providing effective pain relief for those in need.
Collaborating with Patients for Effective Pain Management
Collaboration with patients is a fundamental aspect of effective pain management for pain management doctors. These healthcare professionals must work closely with their patients to develop treatment plans that align with their individual goals, preferences, and values. This may involve discussing various treatment options, setting realistic expectations for pain relief, and addressing any concerns or questions that the patient may have.
In addition to fostering open communication with their patients, pain management doctors must also empower them to take an active role in managing their pain. This may involve providing education about their condition, teaching self-management strategies, and encouraging lifestyle modifications that can help improve their overall well-being. By involving patients in the decision-making process, these doctors can help ensure that treatment plans are tailored to each patient’s unique needs and circumstances.
Furthermore, collaboration with patients also extends to discussing the risks and benefits of narcotic use. Pain management doctors must engage in open and honest conversations with their patients about the potential side effects, risks of addiction, and alternative treatment options. By providing comprehensive information and involving patients in shared decision-making, these doctors can help ensure that narcotic use is managed responsibly and in the best interest of the patient’s overall health.
Addressing the Risks and Benefits of Narcotic Use
Addressing the risks and benefits of narcotic use is a critical responsibility for pain management doctors. While narcotics can provide significant relief for patients suffering from moderate to severe pain, they also carry a risk of abuse, addiction, and potentially life-threatening side effects. As such, these healthcare professionals must carefully weigh the potential benefits of narcotic use against the risks for each individual patient.
In addition to discussing potential risks with their patients, pain management doctors must also implement strategies to mitigate these risks while still providing effective pain relief. This may involve prescribing the lowest effective dose of narcotics, closely monitoring for signs of misuse or diversion, and considering alternative treatment options when appropriate. By taking a proactive approach to risk mitigation, these doctors can help ensure safe and responsible use of narcotics for their patients.
Furthermore, addressing the risks and benefits of narcotic use also involves educating patients about the importance of safe storage and disposal of these medications. Pain management doctors must provide clear instructions on how to store narcotics securely to prevent unauthorized access and how to properly dispose of unused medications to reduce the risk of diversion or accidental ingestion. By empowering patients with this knowledge, these doctors can help minimize the potential harm associated with narcotic use.
The Future of Narcotic Prescribing in Pain Management
The future of narcotic prescribing in pain management is likely to be shaped by ongoing efforts to improve safety and efficacy while still providing adequate pain relief for those in need. This may involve continued research into alternative treatment options for chronic pain conditions, such as non-opioid medications, interventional procedures, and complementary therapies. By expanding the toolkit available to pain management doctors, it may be possible to reduce reliance on narcotics while still effectively managing pain.
Additionally, advancements in technology may also play a role in shaping the future of narcotic prescribing in pain management. Electronic health records, prescription drug monitoring programs, and telemedicine platforms can all help improve communication between healthcare providers, enhance monitoring capabilities, and facilitate safer prescribing practices. By leveraging these technological advancements, pain management doctors can better identify potential signs of opioid misuse or diversion while still providing timely access to effective pain relief for their patients.
Furthermore, ongoing efforts to improve education and training for healthcare professionals may also contribute to the future of narcotic prescribing in pain management. By ensuring that providers are well-informed about current guidelines, best practices, and risk mitigation strategies, it may be possible to reduce the incidence of opioid-related harm while still meeting the needs of patients with chronic pain. Ultimately, by embracing a multifaceted approach that prioritizes safety, efficacy, and patient-centered care, the future of narcotic prescribing in pain management holds promise for improving outcomes for those living with chronic pain conditions.
If you’re interested in learning more about the role of pain management doctors in prescribing narcotics, you may want to check out this article on alzheimerperth.com. This website provides valuable information on various medical topics, including the use of narcotics for pain management. It’s important to stay informed and educated on these matters, especially if you or a loved one are dealing with chronic pain.
FAQs
What is a pain management doctor?
A pain management doctor is a medical professional who specializes in the diagnosis and treatment of chronic pain conditions. They are trained to provide comprehensive care for patients suffering from various types of pain.
Do pain management doctors prescribe narcotics?
Yes, pain management doctors are licensed to prescribe narcotics for the treatment of chronic pain conditions. However, they do so under strict guidelines and regulations to ensure the safe and appropriate use of these medications.
What conditions do pain management doctors treat?
Pain management doctors treat a wide range of conditions, including back pain, neck pain, arthritis, neuropathic pain, fibromyalgia, and other chronic pain syndromes. They also provide care for patients recovering from surgery or injury.
What is the role of narcotics in pain management?
Narcotics, also known as opioids, are a class of medications that are used to manage moderate to severe pain. They work by binding to specific receptors in the brain and spinal cord to reduce the perception of pain.
What are the potential risks of using narcotics for pain management?
While narcotics can be effective in managing pain, they also carry the risk of dependence, addiction, and overdose. Pain management doctors carefully assess each patient’s individual needs and monitor their use of narcotics to minimize these risks.
